Dairy Cattle: More than just “Milk Fever”

– Dr. Shannon Walsh
A Brief Review: Most dairy producers are well familiar with clinical hypocalcemia (milk fever), which looks something like this… A cow is close to calving > calcium demand skyrockets as the cow prepares for colostrum and milk production > at the same time, her dry matter intake drops (=less dietary calcium) > she begins to breakdown bone to release calcium (bone is restored later in lactation) BUT may not be able to do so efficiently (e.g. poor transition diet) or sufficiently (e.g. older, high-producing cows) > calcium is required for muscle function, leading to various symptoms:
- Cardiac muscle > weaker heart contractions, poor circulation > cold ears, etc.
- Smooth muscle
- Gastrointestinal tract rumen stasis, constipation, ↑risk of ketosis, DA
- Reproductive tract > ↑risk of difficult calving and retained placenta
- Skeletal muscle > muscle tremors, wobbly gait, inability to rise
Avoid giving oral calcium boluses to down milk fever cows – the smooth muscle in their esophagus is weak creating a choking hazard.
Calcium is given intravenously and/or subcutaneously and the cow responds well. If 10-15% of cows are affected by milk fever annually, this indicates a herd-level issue and warrants further investigation – e.g. review your dry cow ration with your nutritionist and consult your vet on other preventative strategies.
“Tell Me Something I Don’t Know”…The Finer Points…
- Why isn’t my down cow responding to calcium?
- Can mid-lactation cows be hypocalcemic?
- What is subclinical hypocalcemia?
- Are all oral calcium boluses the same?
1) Why Isn’t my Down Cow Responding to Calcium?
- a) There may be other mineral deficiencies involved besides Calcium (Ca)… (diagnosed by blood test)
Phosphorus (P): Bone is made of Ca, P, and a protein matrix. As bone is broken down to release Ca, P is similarly released and lost from the body via the udder. P is a component of cell membranes and when deficient, muscles and blood vessels are more easily damaged. While P-levels tend to restore themselves after Ca is provided, research has shown that including it in down cow therapy can increase success.
Magnesium (Mg) & Vitamin D: Both are involved in complex pathways that regulate blood calcium. Low levels of Mg and VitD are not directly related to milk fever but rather prevent the cow from efficiently releasing stored Ca from bone, reducing the loss of Ca in urine, and absorbing dietary Ca. Deficiencies in Mg & VitD are uncommon.
Did you know…?
The phosphorus in “Cal-Plus” (blue-top) are ‘phosphites’ which are NOT biologically available to the cow. Enemas or *oral phosphorus boluses* contain biologically available ‘phosphates’ (*new*).
Do NOT mix phosphorus enemas with calcium solutions (e.g. Cal-Plus, Cal-Boro). The phosphorus (phosphate) and calcium will bind and precipitate out of solution, rendering the treatment useless and causing stress on the cow’s kidneys.
Potassium (K): Unrelated to milk fever but involved in muscle contraction, low K can result in muscle weakness. A mild K deficiency is common in cows off feed, but we don’t typically observe K-levels low enough to see symptoms or warrant treatment.
 b) She may also have an injury…
b) She may also have an injury…
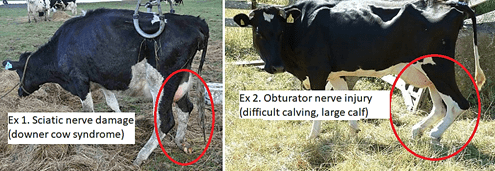
Due to her weakened or uncoordinated state a hypocalcemic cow may injure herself when she initially goes down or during her attempts to rise – e.g. soft tissue injuries, dislocations, or fractures.
A pelvic nerve injury from a difficult calving or delivery of a large calf may also cause or exacerbate hind end weakness and paralysis. Additionally, if the cow has been down for more than 24hrs, the pressure of her body weight prevents adequate circulation of oxygen to her muscles and nerves resulting in permanent damage (a.k.a. compartment syndrome or downer cow syndrome). Likelihood of recovery from ‘downer cow syndrome’ may be gauged with a blood test that measure enzymes (proteins) that are released from damaged muscle cells.
c) She may have an additional illness… There is a correlation between the presence of bacterial toxins in the blood and low blood calcium. While the underlying mechanism is beyond the scope of this article (and under some academic debate), a cow affected by toxic mastitis, metritis, or enteritis (gastrointestinal infection) will also often be low in calcium. In these cases, calcium may be given as a supportive therapy, but treating her infection is critical.
Milk fever is one of the most studied and most complicated diseases in dairy cattle. The condition has been under study for >200 years, and while there has been tremendous progress in our understanding of this condition, there are still gaps in our knowledge.
2) Can Mid-lactation Down Cows be Hypocalcemic? > Yes. For example,
- Toxemia-associated hypocalcemia: described above.
- Estrus-associated hypocalcemia: high levels of estrogen following a strong heat can interfere with the release of calcium stores from bone.
- Breed-predisposition: atypical cases of hypocalcemia are more common in Jerseys.
3) What is Subclinical Hypocalcemia (SCH)?
- Blood calcium levels are below normal, but not sufficiently low to cause muscle weakness/down cows
- Unlike clinical hypocalcemia, it is common and as likely in heifers as in older lactations
- May be transient (<3 days) or chronic (>3 days). Impacts may include the following (more research needed):
- Transient SCH – reduced pregnancy rate at first service
- Chronic SCH – higher SCC and lower milk components in early lactation, increased risk of transition cow diseases (retained placenta, mastitis, ketosis, etc.), slower return to cyclicity and reduced pregnancy rate at first service
Prevention is achieved by use of oral calcium boluses at freshening – either as 1) blanket therapy to all Lactation 2+ cows, or 2) selectively to lame and high-producing cows.
4) Are All Oral Calcium Boluses the Same? > No. Note: At Upper Grand Vets, we do not promote one manufacturer over another. Rather, we offer products that balance economic value with evidence-based medicine. Although oral calcium boluses from different manufacturers are generally similar, we recommend verifying that the product you use meets the following criteria:
- Contains calcium in two forms: rapid-release (e.g. calcium chloride) and longer-release (e.g. calcium sulfate)
- Lists a protective coating (often xanthan gum) that protects the esophagus from irritation (calcium is caustic)
- Caution: Do not use broken boluses, as the protective coating has been compromised. Most manufacturers will replace these at no charge.
If you have any questions on these or other topics, please do not hesitate to contact one of our Veterinarians.




